Abstract

Background:
Superior Vena Cava (SVC) Syndrome (SVCS), defined by obstruction of blood flow through the SVC, is commonly caused by a mediastinal tumor (i.e. malignant SVCS, m-SVCS). Little is known regarding co-existing SVC thrombosis at diagnosis in this high risk setting. Anticoagulation (AC) is often utilized even in the absence of thrombosis or stents, but evidence is lacking.
Aims:
1) To determine factors associated with thrombosis and AC at m-SVCS diagnosis; 2) To evaluate the effect of baseline AC and SVC thrombosis on outcomes.
Methods:
The electronic records of 2 academic medical centers in Israel were screened for diagnostic codes compatible with SVCS and malignancy between 2007 and 2015. Patients were included if they had active cancer and m-SVCS reported in chest computerized tomography (CT) with intravenous (IV) contrast medium. Records were followed from m-SVCS diagnosis for 6 months.
Baseline patient, cancer and m-SVCS-related characteristics were collected. AC use and endovascular SVC stent placement were recorded throughout the study. Accessible diagnostic and follow-up IV contrast CTs were reviewed by two radiologists to confirm m-SVCS diagnosis and evaluate thrombosis. The primary endpoint was death from any cause. Secondary endpoints included new/recurrent SVC thrombosis. Baseline variables that had a statistically significant association with baseline thrombosis or death on univariate analysis were entered into a General Linear Model and multivariable cox regression model, respectively, for multivariable analysis. Significance was set at p < 0.05.
Results:
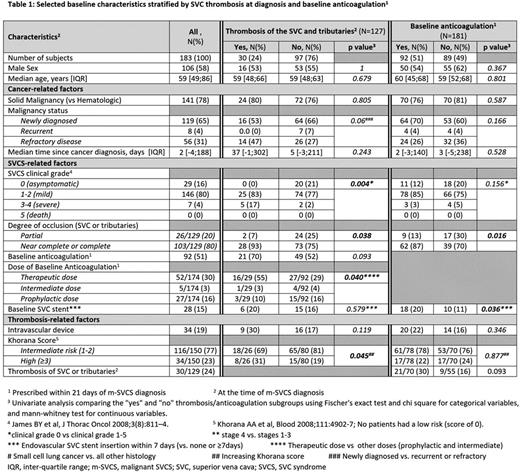
The cohort included the 183 patients, 70% (129) of whom had a reviewable baseline CT. Baseline characteristics are shown in Table 1. Briefly, 65% (119/183) had newly diagnosed cancer of any histology, 22% (40/183) had hematological malignancy (mainly aggressive lymphoma), and 16% (29/183) had no symptoms attributable to m-SVCS (i.e. clinical grade 0). Thrombosis of the SVC or tributaries at diagnosis was seen in 24% (30/127). Baseline AC (within 21 days of m-SVCS diagnosis) was used in 51% of patients for a median duration of 68 days [range: 14-179]. Thirty percent of thrombotic cases received no AC, while 52% of non-thrombotic cases received AC at varying doses. Patients receiving baseline AC were more likely to have had a SVC stent placed at baseline, and had higher grade venous occlusion and a trend to more thrombosis of SVC and tributaries (univariate analysis; Table 1). On multivariate analysis, only symptomatic m-SVCS (P<0.01) and increasing Khorana score (p<0.05) were associated with baseline thrombosis (univariate analysis shown in Table 1).
Over a median FU of 44 [IQR 22-93] days, 49% (90/182) of patients died. A follow up CT was performed in 61/129 (47%) patients at a median of 138 days [IQR 71-182] from diagnosis, 30% (18) of whom died. New thrombosis of SVC and tributaries was identified in 10/61 (16%) at a median of 74 days [IQR: 53-150]. Patients with baseline AC had thrombosis on follow-up CT in 21% of cases (8/40) compared to 10% (2/20) in those without baseline AC (p=0.471). Among the 68/129 without a follow up CT, 45 (66%) died over a median follow up of 72 days (IQR 23-182).
In time dependent cox analysis, baseline AC (compared to none) was not associated with risk of death (HR 0.85; 95% CI 0.55-1.29). In multiple regression analysis of baseline variables, increasing age (HR 1.04, 95% CI 1.02-1.06), malignancy stage IV (HR 4.57, 95% CI 2.29-9.13) and refractory cancer (HR 1.95, 95% CI 1.17-3.25) were associated with death.
Conclusion:
Thrombosis of SVC and tributaries is a common complication of m-SVCS, and is associated with symptomatic presentation and a high Khorana score. Prognosis in m-SVCS is dismal and appears to be determined by the prognosis of the underlying cancer and responsiveness to prior anticancer therapy and not by the presence of thrombosis at diagnosis. The high early death rate, low numbers of thrombotic events and confounding by AC indication, preclude ruling out a role for AC in selected cases. We propose that therapeutic dose AC in thrombotic m-SVCS and prophylactic AC in non-thrombotic m-SVCS be evaluated prospectively in newly diagnosed patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal